Researchers have developed bioprinted blood vessels using human cells to better understand and treat aggressive brain tumors like glioblastoma. This approach aims to replicate the brain’s vascular networks more accurately, providing a better platform for studying tumor behavior and testing therapies.
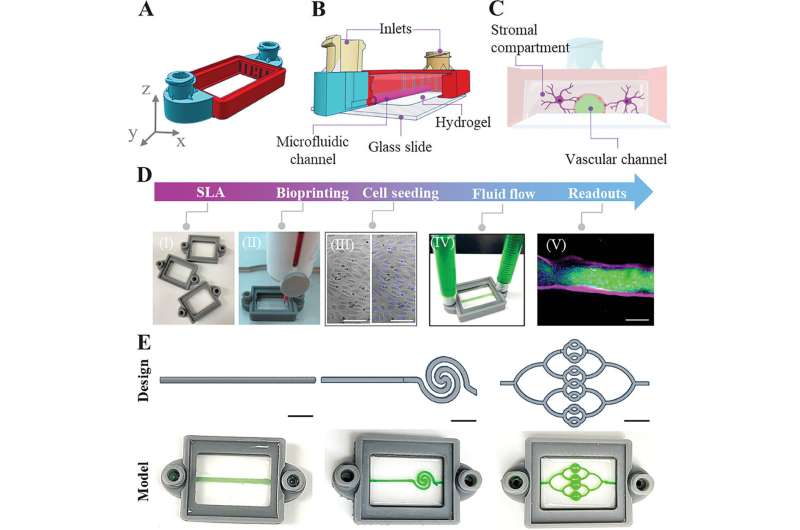
Fig: llustrating the Assembly of a 3D-bioprinted System. Credit: Advanced Healthcare Materials (2024). DOI: 10.1002/adhm.202401876
Challenges with Glioblastoma
Glioblastoma is a fast-growing and deadly brain cancer. One major challenge in treating it is the blood-brain barrier, which protects the brain but also prevents many drugs from reaching tumor cells.
Advancement in Bioprinting
The team used advanced bioprinting technology to create detailed blood vessel structures that closely mimic the unique features of brain vasculature. Traditional models often fall short in replicating the complex environment of the brain’s blood vessels. By using bioprinting, researchers can produce vessels with the same cellular composition, three-dimensional structure, and mechanical properties as those found in the human brain.
Why These Vessels More Closely Mimic Brain Vasculature
Brain blood vessels have distinct characteristics, such as tight junctions between endothelial cells, a specific basement membrane composition, and interactions with surrounding neural cells. The bioprinted vessels incorporate these features by using brain-specific endothelial cells and incorporating extracellular matrix components native to brain tissue. This results in a model that more accurately represents the physiological conditions within the brain, including the critical blood-brain barrier.
Studying Differences Through Various Geometries
By altering the geometries of the bioprinted vessels—such as changing the diameter, curvature, and branching patterns—researchers can study how these physical differences affect tumor growth and drug delivery. Different geometries can influence blood flow dynamics, shear stress on vessel walls, and the diffusion of molecules, all of which impact how tumor cells interact with their environment. For instance:
- Vessel Diameter: Smaller vessels may restrict the movement of larger therapeutic agents, affecting their ability to reach tumor cells.
- Branching Patterns: Complex branching can create regions of low blood flow, where tumor cells might thrive due to reduced oxygen and nutrient levels.
- Curvature and Tortuosity: Curved vessels can alter shear stress, influencing endothelial cell behavior and potentially affecting tumor cell adhesion and invasion.
By experimenting with these variables, scientists can observe how glioblastoma cells respond to different vascular environments, leading to a better understanding of tumor behavior.
Implications for Future Treatments
Using these more accurate bioprinted vessels, researchers can test drugs and therapies under conditions that closely resemble the human brain. This could lead to the development of treatments that can effectively cross the blood-brain barrier and target tumor cells more precisely. The technology also opens possibilities for personalized medicine by using a patient’s own cells to create customized vascular models for testing.
Next Steps
Future research will focus on refining the bioprinting process to include even more complex features of brain vasculature, such as pericytes and astrocytes that interact with blood vessels. Integrating components of the immune system may also provide a more comprehensive model for studying not just glioblastoma but other neurological diseases as well.

Leave a comment