Regenerative cell therapy aims to repair or replace damaged tissues using living cells. However, traditional methods for delivering these therapeutic cells—like injecting them directly into a patient—often face challenges. Issues like cell survival, retention in the targeted area, and integration with existing tissues limit the effectiveness of these therapies. Biofabrication techniques are emerging to address these barriers by offering more reliable and precise ways to deliver therapeutic cells. In a recent Science perspective Dr. Yu Shrike Zhang, Dr. Alireza Dolatshahi-Pirouz, and Dr. Gorka Orive discuss the potential value in-situ bioprinting can have on cell therapeutics for patients in the near future.
Advancements in 3D Bioprinting
3D bioprinting, also known as additive biomanufacturing, has enhanced the field of tissue engineering by enabling precise spatial arrangement of cells and biomaterials to replicate natural tissue structures. Techniques like extrusion bioprinting, inkjet bioprinting, and vat-polymerization allow scientists to layer cells and biomaterials into complex 3D structures, achieving levels of precision that traditional methods lack. These modalities offer new possibilities for creating both biomaterial-enriched and biomaterial-free cell structures that more closely mimic native tissues.
In Situ Bioprinting: Building Tissues Directly in the Body
Another biofabrication method, in situ bioprinting, builds tissue structures directly at the therapeutic site, inside the patient’s body. This approach avoids the need for external construction and transplantation, reducing contamination risks, improving cell survival, and facilitating smoother integration with the body’s tissues. In situ bioprinting is particularly promising for emergency scenarios—such as battlefield injuries—where on-the-spot tissue repair is essential. It allows for precise alignment with the natural architecture of the target site, offering applications across various medical needs.
Techniques for In Situ Bioprinting
Several innovative techniques are being explored for in situ bioprinting:
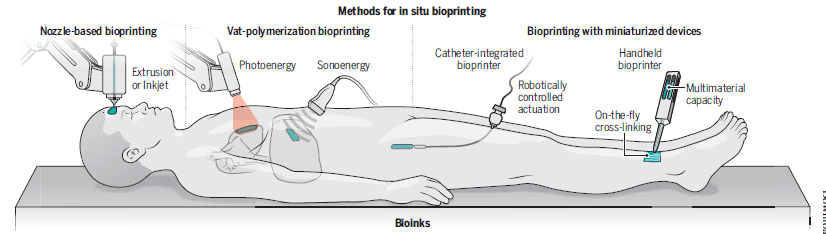
Figure 1: Methods for in situ bioprinting in regenerative medicine, illustrating various techniques such as nozzle-based bioprinting, vat-polymerization, catheter-integrated, and handheld bioprinters. From Zhang, Dolatshahi-Pirouz, and Orive, Science, 2024.
- Nozzle-Based Bioprinting:
- Extrusion or Inkjet Bioprinting: Uses a nozzle to deposit bioinks at the target site with precision, often applied to create structured tissue layers.
- Vat-Polymerization Bioprinting:
- Photoenergy: Solidifies bioinks layer by layer using light within a vat, forming detailed 3D structures.
- Sonoenergy: Shapes bioinks using ultrasound waves, enabling the construction of tissue structures with sound-based technology.
- Bioprinting with Miniaturized Devices:
- Handheld Bioprinter: A portable device that allows surgeons to directly print bioinks onto wounds or target sites, providing flexibility in positioning.
- Catheter-Integrated Bioprinter: Uses a miniaturized, catheter-based printhead controlled robotically to deliver bioinks precisely to deep or hard-to-reach areas, ideal for minimally invasive procedures.
- On-the-Fly Cross-Linking: Enables real-time hardening or setting of bioinks during the printing process, ensuring structural stability immediately.
- Multimaterial Capacity: Capable of printing multiple types of bioinks in one session, allowing complex tissue compositions and structures to be built.
Each method can produce customizable tissue structures tailored to the unique needs of each patient, facilitating higher adaptability and aesthetic outcomes.
High-Density Bioinks and Biomaterial-Free Constructs
One of the major advancements in in situ bioprinting is the use of high-density bioinks that contain only cellular components, such as spheroids or organoids. These bioinks can replicate the densely packed cellular arrangements found in native tissues. As high-density bioinks mature, they allow for strong cell-to-cell interactions, promoting natural tissue formation. These biomaterial-free constructs bring us closer to creating functional tissue replacements for organs like the liver or heart, where high cell density and organization are crucial.
Future Possibilities and Challenges
While in situ bioprinting holds immense potential, it is not without its challenges. For instance, bioprinting dense cellular structures directly into a patient requires precise adhesion with surrounding tissues and may call for additional growth factors or bioactive agents to support cellular integration. Moreover, the technology still faces hurdles in ensuring the longevity and functionality of printed tissues. Future improvements may integrate AI-driven algorithms and controlled-release biomaterials, enabling precise patterning and on-site cellular modification.
The integration of 3D bioprinting and regenerative medicine is has promise to bring novel application to market. By overcoming the limitations of traditional cell therapy with precise biofabrication techniques, researchers are unlocking new possibilities for tissue repair and replacement. As in situ bioprinting continues to advance, we move closer to a future where bioengineered tissues can seamlessly restore function and appearance in damaged areas, opening new doors for personalized regenerative therapies.
Find the perspective Science paper here.

Leave a comment