As we think about where bioprinting can truly start playing a role in implants, we naturally ask, “which tissue type will we first see become implanted?” While skin, might have been the choice we thought of about 15 years ago, as history as played out, bone is actually at the forefront of the industry. We have actually begun to see some fascinating examples of prints make it safely into patients and have real value for them. As we think about how we got here, we think about the chemistries really that have guided us to this point. First there was the belief that polycaprolactone(PCL), would be a main driver of allowing us to see successful regenerative bone implants. One of the most exciting developments was when DePuy Synthes acquired, Tissue Regeneration Systems Inc. (TRS) back in 2017 for their host of technologies. Particularly though, there was much attention given to the PCL printing that was being done by TRS. As we’ve seen, the technology never took off, as PCL seemed to be too brittle as the backbone material and to date has not been integrated as a full product in the DePuy product portfolio. So, if bone is so far ahead, and PCL backbone wasn’t the answer, what are the chemistries that are driving this forward?
The answer lies in 2 chemistries: hydroxyapatite and β-TCP, and particularly 3 companies at the forefront: Dimension Inx, Cerhum, and Ossiform.
Chemical Backbones
Hydroxyapatite, a naturally occurring mineral form of calcium apatite with the chemical formula Ca₁₀(PO₄)₆(OH)₂, was first identified and named in the 19th century. Its chemical structure and composition were studied in depth, establishing it as a major component of bones and teeth. In the mid-20th century, researchers began exploring hydroxyapatite for biomedical applications due to its excellent biocompatibility and similarity to human bone mineral. It was recognized for its ability to integrate with natural bone tissue without causing adverse immune reactions. By the 1970s and 1980s, hydroxyapatite gained prominence in orthopedic and dental implants. Surgeons utilized HA coatings and implants to enhance bone repair and promote osseointegration, particularly in joint replacements, dental implants, and bone grafts.
Likewise, β-TCP, with the chemical formula Ca₃(PO₄)₂, emerged as a synthetic bioceramic material in the late 20th century. It was developed as a biomaterial due to its biocompatibility and ability to support bone regeneration. Since its inception, β-TCP has been extensively studied and used in orthopedic and dental surgeries. It is recognized for its osteoconductive properties, meaning it provides a scaffold that facilitates the attachment and growth of bone cells. β-TCP is commonly used as a bone graft substitute in medical procedures. Its resorbable nature allows it to gradually degrade in the body while being replaced by natural bone tissue over time.
Hydroxyapatite and B-TCP have had a long history in the field of dental and orthopedic implants. They have become staples of use as they are both highly accepted materials to use, as well as found in a variety of applications, such as paste, coatings, and putties. The trick has been understanding these first off have great regenerative capabilities and tunable biodegradable profiles.
Using this idea as a starting point, companies have been learning ways to pattern these materials and this is where the significance of our view lies. Companies have been using different 3D printing methods to be able to shape these materials in relevant micro- and macro- geometries for better personalized bone regeneration. Let’s dive into those companies:
The first company, founded by Adam Jakus and Ramille Shah in 2016, which we have mentioned before is Dimension Inx. They really began to make waves when they publish a key paper in Science that spoke about what they term 3D paints. They are inks made in trisolvent mixture that allows ink to be pasty and harden when the solvent dissolves after printing. In the Science paper, they described their hyperelastic bone as a 9:1 ratio of HA to PLGA. The two things to note here are that first off it is an HA driven backbone material. The second is that given it is pasty they could print it out into lattice layers through FDM dispension, and these specific lattices enhance the regenerative capabilities of the material. The microarchitecture enhances the therapeutic at the same time giving the option to have macroarchitecture specificity to fit a patient’s need.
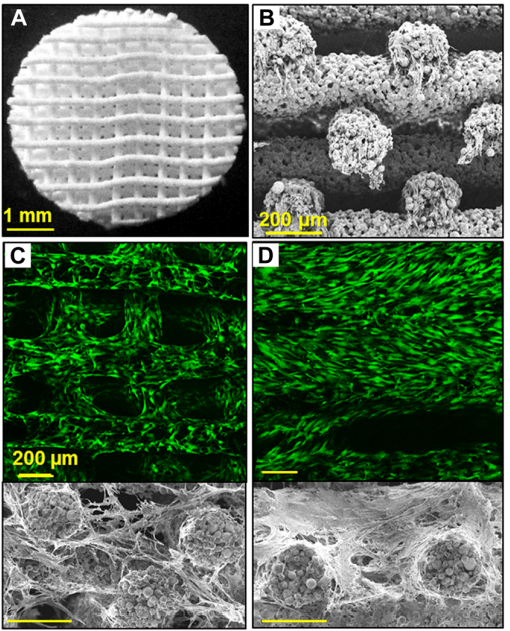
Figure 1 – from their original Science paper showing their ability to lattice print the material.
To date hyperelastic bone is now called CMFlex and has been 510k approved. And it is also beginning to be used in patient’s. Now the next challenge for Dimension Inx will be to ensure adoption and commercial success as a product.
Cerhum was created in 2015 by Grégory Nolens as a spin-out from Sirris, the Belgian national Science and Technology Institute. The company’s technology works by using SLA technology to print their biomaterial, which is then sintered to be a fully HA material. Although the print does have to be post-bake in a sintering process, given the material is printed using SLA, they are able to make complex geometric patterns otherwise not possible on FDM.
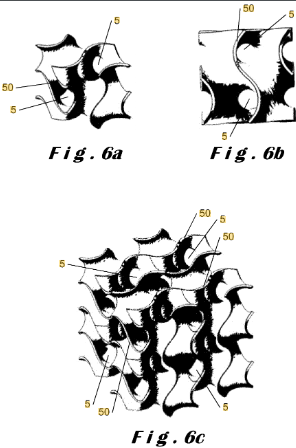
Figure 2 – shows the intricate pattern able to be achieved using SLA that claims to enhance osteoconductive regeneration taken from Cerhum patent.
To date the material has been approved in Europe and also has begun to be used in patient. Their most recent publication lead by Dr. Lucian Vidal, shows how 13 patients benefited from the technology. They are received fully custom bioactive implants that are projected to restore bone.
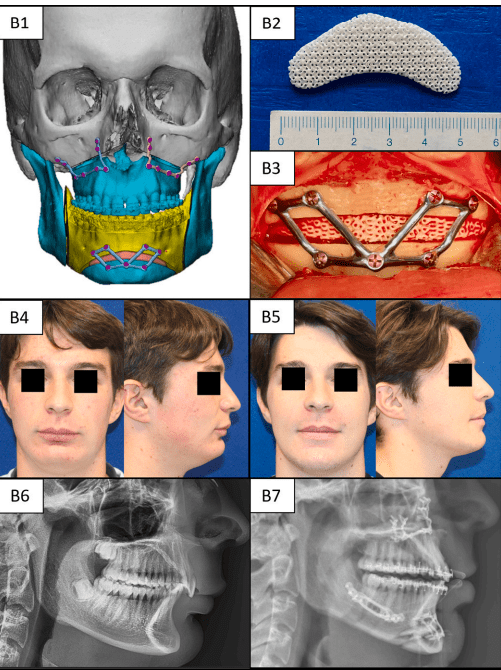
Figure 3 – taken from the recent Cerhum publication shows how digitally planning is used and the HA implant is use alongside a reinforced titanium one to create an enhanced therapeutic outcome.
The next steps are to see the long term affects and to create further viable commercial directions for the technology.
Ossiform was a company founded in 2018 by Mette Ruge, Mogens Gedary, Peter Thomsen, and Emil Anderson. The technology was developed at the University of Southern Denmark. The foundation of the method is based off of extruding a paste using FDM then sintering the material. They have moved to focus specifically on β-TCP stating that it has better osteoconductive properties and term the product P3D Bone. The technology is still developing given they are still waiting for their 510K approval and have yet to implant into patients. They do have promising initial pre-clinical data.
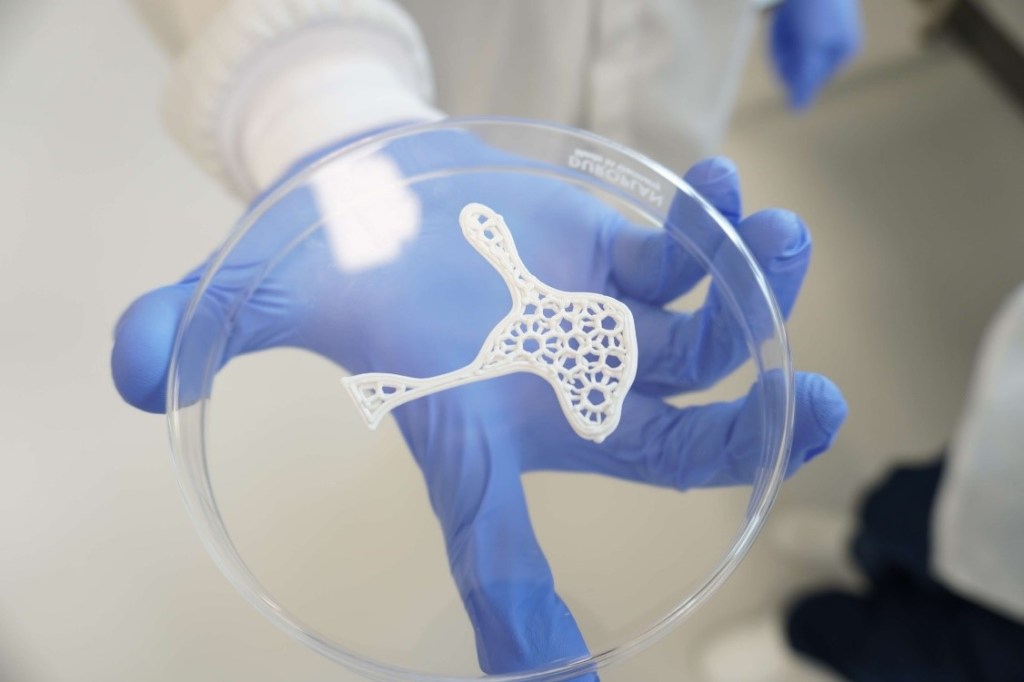
Figure 4 – an image of one of their P3D prints from their website using FDM printing.
Conclusion
For those that say 3D bioprinting is years away, you can use these examples as proof that the industry has arrived. These are real companies, treating real patients, that are valuing from materials enhanced by 3D printing to give superior osteoconductive properties. While, follow up of these patients will be required to see how they perform, there is a plethora of data that supports these patients will do well in years to come. On the other hand, these companies particularly those serving patients already will need to drive for partnerships to gain greater commercial access. As it has been seen in the past with the history of Organogenesis, it’s not just how good the technology is, but also how well it can be commercialized. I hope this gives some insight though to some leading examples on the rate to control HA and β-TCP .

Leave a comment